From Personal Tragedy to Life Purpose: How One Masters Student at Mount Sinai Was Inspired to Focus on a Career in Public Health
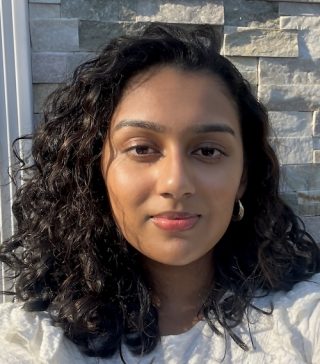
Brianna Sukhdeo, a second year Master of Public Health student
Brianna Sukhdeo is a second year Master of Public Health (MPH) student in the Health Promotion and Disease Prevention concentration. She is also the first student from the Icahn School of Medicine at Mount Sinai to be selected as an ambassador as part of a special program administered by the Association of Schools & Programs of Public Health.
This honor is just the next step for her as she embarks on a career in public health.
She had been inspired to study public health during the onset of the COVID-19 pandemic as she watched her mother having trouble getting proper medical care. As soon as she arrived at Mount Sinai, she began pursuing opportunities outside the classroom to purse this goal.
For example, she has been working with Lauren Zajac, MD, MPH and Sofia Curdumi Pendley, PhD, MPH, on TEAM Kids (Team-based Environmental Asthma Management), a pediatric asthma clinic at Mount Sinai.
She found that mentors were willing to invite students into professional spaces to give them networking experiences and to develop new skills. Her mentors have been responsive to outreach from students and are willing to share professional opportunities, even to mentees they don’t work with directly.
The team that manages the Graduate Program in Public Health recognized that she would be a good fit for the This is Public Heath (TIPH) Ambassador Program run by the Association of Schools & Programs of Public Health. So they met with her to explain the opportunity and then nominated her for it.
“I was excited to learn that I would be the first representative from Mount Sinai to participate,” she says of the program, which aims to raise awareness of the field of public health to students across the United States.
Embarking on a career in public health wasn’t always her primary goal.
“I want students to understand how foundational public health is to health care careers, along with how to make connections between this field and industries such as business, law, politics, and environmental science,” she says. “Public Health should be the lens through which we view health in our society.”
While completing her undergraduate degree in psychology, she thought about becoming a school psychologist or child psychologist. Her plans changed when her mom got sick and was hospitalized during the COVID-19 pandemic. She saw how her mother wasn’t getting the care she needed and how resources were diverted during the pandemic.
Her mother had been living with liver problems and had been treated at other hospitals without a specific diagnosis. She finally came to The Mount Sinai Hospital, and her daughter credits this with saving her mother’s life. Her mother was diagnosed and treated for autoimmune hepatitis, a chronic liver disease. She has since recovered.
During the pandemic, Brianna Sukhdeo was inspired to help patients who were alone in hospitals due to COVID-19 restrictions, which led her to an internship at the Stony Brook University Emergency Department helping patients and families in the Emergency Department. Her supervisor, Samita Heslin, MD, MPH, MBA, was an Emergency Department doctor. “She explained how useful and versatile public health is in addressing the foundational issues of health and how these concepts can be applied to patient care,” she says.
While researching the next step in her educational journey, Brianna discovered many pediatric mentors were available at Mount Sinai.
“I was drawn to the fact that the Icahn School of Medicine was within the Mount Sinai Health System, which provides many opportunities for professional development, such as volunteering in clinical settings, research, and quality improvement,” she says.
“I often work with medical students, health administration students, and students from several other programs,” she says of her time at the Icahn School of Medicine. “The collaborative environment encouraged me to be an active participant as a student instead of just passive learning.”
After graduating from the MPH program in June, she hopes to attend medical school and become a public health pediatrician.
The goal of the This is Public Health Ambassador Program is to raise awareness of the field of public health. She believes this is crucial because she didn’t know much about the field until she was far into her academic journey.
“I want students to understand how foundational public health is to health care careers, along with how to make connections between this field and industries such as business, law, politics, and environmental science,” she says. “Public Health should be the lens through which we view health in our society.”
The TIPH Cohort runs from August through June, and the most important part of the experience is the networking. Participating schools have the chance to nominate one student a year. They meet once a month to discuss the similarities and differences of their programs, places of need, and to share resources. Brianna has enjoyed learning about the policy differences from ambassadors at schools in other states.
The TIPH Cohort provides advice to prospective public health students, such as why to study in this field, how to pick a school, how to successfully apply to programs, and more. Brianna has attended virtual and in-person recruitment fairs to answer these student questions. Each TIPH Cohort participant completes a presentation or project, which can include interviewing professionals in the field, educating students about public health topics, and more.



 Before COVID-19 was even formally recognized as a pandemic, David L. Reich, MD, President of The Mount Sinai Hospital, was hearing from his anesthesiologist peers in Europe about a terribly problematic “respiratory disease” with a high mortality rate.
Before COVID-19 was even formally recognized as a pandemic, David L. Reich, MD, President of The Mount Sinai Hospital, was hearing from his anesthesiologist peers in Europe about a terribly problematic “respiratory disease” with a high mortality rate.

