Updated on Apr 25, 2025 | COVID-19 Reflections, Featured, Research

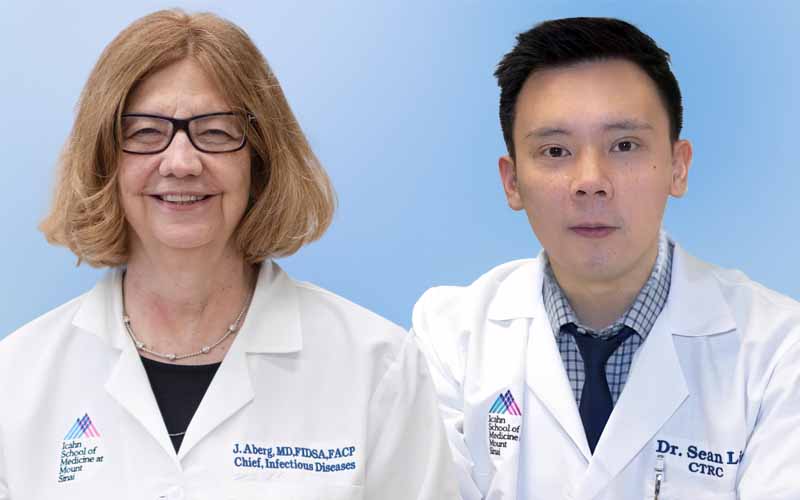
Nicole Simons, MA, right, with Katherine Keller, Clinical Research Coordinator
When the first of several waves of COVID-19 cases hit New York City, Nicole Simons, MA, had just landed her first big job out of school as a research coordinator at the Icahn School of Medicine at Mount Sinai. In a matter of days, her dream job was eliminated, along with the jobs of several colleagues.
Then came the call from Human Resources: Could she take on a front-line job that would expose her to this unknown virus and clinics filled with COVID-19 patients? Her answer was a resounding yes.
In a moment of instant serendipity, she was reassigned to work for Alexander Charney, MD, PhD, a noted researcher in the field of schizophrenia, a disease that had first captured her attention in college.
Working closely with clinicians on the front lines during the pandemic would turn out to be a lifechanging experience. She visited hospital wards to collect samples, helped out staff when she could, and even served as a second author of a paper in Nature Medicine that described the team’s work. Now she is the Program Manager of the Jeff and Lisa Blau Adolescent Consultation Center for Resilience and Treatment and is a PhD student in the Clinical Research Program at the Icahn School of Medicine, with plans to continue research into the genetics of schizophrenia. “Working with clinical colleagues on the frontlines really got me thinking about how to narrow the gap between research and clinical care. I plan to use the lessons I’ve learned to keep building research programs that move us closer to becoming a true learning health care system.”
It’s a long way from those early days of the pandemic in 2020. Dr. Charney, Associate Professor, Psychiatry, and Genetics and Genomic Sciences, had been asked by hospital leadership to rapidly build up a COVID-19 Biobank that would collect hundreds of blood samples from patients hospitalized with COIVD-19. It would ultimately serve as a backbone for ongoing research into the virus and the human immune response.

Nicole Simons, MA
Dr. Charney’s team consisted of 100 volunteers who, like Ms. Simons, had seen their research projects paused but were given a chance to come help. The team quickly designed a sample-collection protocol, and once this was in place, the cadre of volunteers organized itself into six teams, with Ms. Simons assigned to the “Running Team.” This team was responsible for transporting collection kits to every location within the hospital, and then bringing those kits back.
What might sound like a simple and straightforward assignment involved a major hurdle. How to gain access to clinics where new hospital rules would not even allow families to enter, even when patients were seriously ill? Ms. Simons would have to find a way in.
“Entering those clinics was like entering a fog of war environment. The strain on the nurses and doctors was palpable; we needed to visit their clinics without creating additional work for them” she says. They had to figure out a way to make easy for them to know if they should allow the researchers on the floor.
“I came up with this idea of making our research team stand apart so we’d be instantly recognizable.” Her solution: hot pink everything. “We wanted to stand out, so we wore hot pink scrubs, gloves, hairnets. Even our labels were pink,” she says. She and her teammates quickly developed a rapport with the nurses managing the floors they’d visit at all hours of the day and night.
“I felt like we were on the outside looking in, that we were somehow protected bystanders while they provided round-the-clock, unconditional care for their patients. To say thank you and support them, we brought them candy and other treats,” she says. They heard that nurses working in the tents constructed in Central Park needed clean, dry socks, so they asked for sock donations, and the response was instantaneous.
Lending help to the clinicians working in the hardest of circumstances also perpetuated for her a sense of shared purpose with staff and faculty at Mount Sinai. Among the volunteers at the Biobank, she found strength.

During the pandemic, Nicole Simons, MA, left, and a team collected hundreds of blood samples from patients hospitalized with COIVD-19, working with MIriam Merad, MD, PhD, center, Dean for Translational Research and Therapeutic Innovation, and Alexander Charney, MD, PhD,
“We all shared this common goal to collect those samples, no matter the hurdles. When the hours were long, and the days were hard, we had this shared humanity that pulled us through,” she says.
When the team reached its goal of 500 samples, they pushed on, ultimately sampling more than 700 participants in 49 days, amounting to more than 10,000 vacutainers portioned into 50,000 smaller samples. A high level of organization was critical to success.
“But strong morale, in the darkest of times, was what really got us through those long days,” she says. “At such a difficult time, it felt like a huge stroke of luck to be working for Dr. Charney, a psychiatrist, leading the Biobank team. His commitment to resilience and mental health was non-stop. He created a safety net for us, with regular weekly check-ins and the option for one-on-one counseling with him any time.”
In July 2020, she served as second author of a paper published in Nature Medicine describing the Biobank’s unique 49- day deep dive to uncover the pathogenicity of the virus. The authors would describe their journey as “not necessarily a model to follow, but rather a live-and-learn memoir of our actions and mistakes under uniquely strenuous circumstances.”
“The team was working intensely in a very high stress, high stakes environment, without much preparation for what we would all come to realize was a once in a lifetime experience,” says Dr. Charney, now Director of The Charles Bronfman Institute for Personalized Medicine and Vice Chair of the Windreich Department of AI and Human Health. “Their mental health was front and center for me. What pulled them through, I believe, was their strong purpose and being part of the group that didn’t have to stay home.”