New Curriculum for the Master of Science in Biomedical Science Program Provides More Options for Students
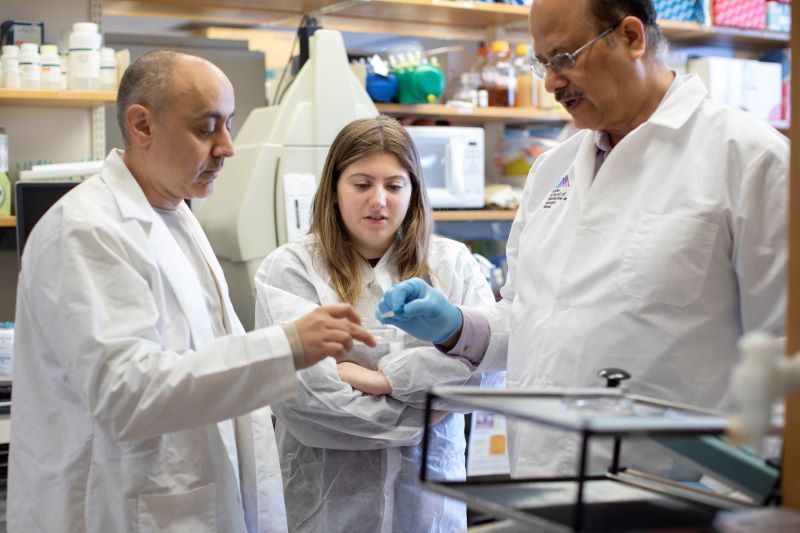
Jose Silva, PhD, left, Program Director, Master of Science in Biomedical Science, and Professor, Pathology, Molecular and Cell Based Medicine, and Oncological Sciences, shown in his lab.
The Graduate School of Biomedical Sciences, part of the Icahn School of Medicine at Mount Sinai, has announced a new curriculum structure for its Master of Science in Biomedical Science (MSBS) program.
The MSBS program, started in 2005, features the multidisciplinary research education available at the school, a commitment to translating fundamental biomedical research into disease prevention and novel therapies, and a dedication to preparing students to contribute to the biomedical enterprise in the non-profit or for-profit sectors.
The program prepares students for a range of health-related advanced degree programs and careers, whether focused on medicine, such as the MD program; research, such as the PhD and MD-PhD programs; or manager-level employment in the clinical and industrial sectors. Eligible students should have a degree in science or a related discipline from an accredited college or university.
“For 20 years, our MSBS program has successfully prepared our students for future success in advance degree programs. Nonetheless, we recognized that a changing job environment required us to provide students with more options, and the new program structure does just that,” says Eric Sobie, PhD, Senior Associate Dean for Master’s in Basic Science Programs.
The program has been restructured to address the changing educational landscape. The new MSBS program offers four distinct tracks that target different types of students and provide greater flexibility for how students can complete the program. The total minimum credits has been reduced from 45 to 36 credits over two to four semesters.
Students will choose their track based on their career goals and stage of life:
- Track 1: Post-Baccalaureate Pre-doctoral (pre-PhD or pre-MD-PhD): This full-time, four-semester track requires students to complete a master’s thesis based on original laboratory research and features a staggered block schedule to facilitate focused study. Students will learn the fundamentals of biomedical sciences while engaging in hands-on research in the laboratories of their chosen Principal Investigators.
- Track 2: Post-Baccalaureate Pre-medical (pre-MD): This full-time, three-semester track also follows a block schedule structure. Students graduate with a capstone project and a final comprehensive examination. This track allows students interested in applying to MD programs to better prepare for the MCAT exam by offering a lighter course load during the spring semester. Students also benefit from non-curricular experiences available at The Mount Sinai Hospital, such as clinical shadowing.
- Track 3: Industry/Clinical/Professional Development: This flexible track, available in three or four semesters, combines a block schedule alongside a capstone project. It caters to individuals working in the clinical, educational, or private sector who aim to enhance their skills and advance their careers into higher-ranked, better-paid positions.
- Track 4: Accelerated Industry/Clinical/Professional Development: This faster-paced version of Track 3 consists of two full-time semesters with a block schedule, a capstone project and a final comprehensive examination. It is designed for individuals seeking to enhance their skills within a condensed time frame.
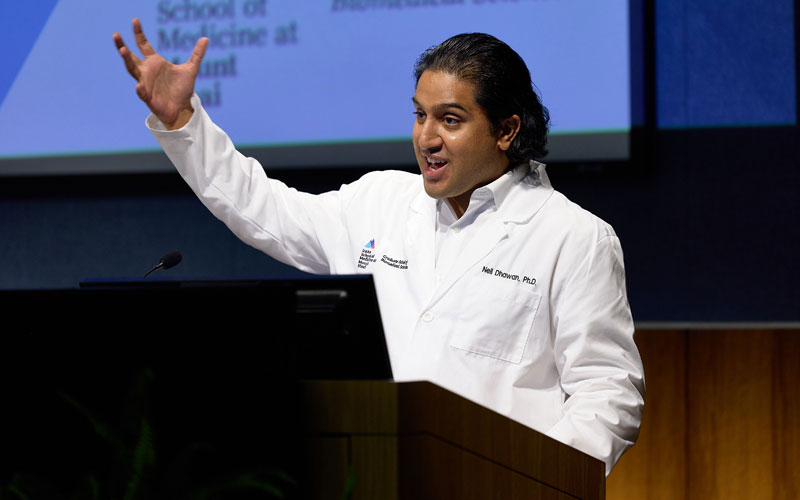
“Our new curriculum retains our unique hands-on training while offering more options and flexible tracks to support your career goals. Whether you’re interested in research, healthcare, or industry, and whether you’re a recent graduate or a professional looking to advance, we’re committed to helping you gain the knowledge and experience needed to take your career to the next level,” says Jose Silva, PhD, MSBS Program Director and Professor, Pathology, Molecular and Cell Based Medicine, and Oncological Sciences.
These tracks will continue to leverage the multidisciplinary training areas available at the Icahn School of Medicine at Mount Sinai through the PhD programs in Biomedical Sciences, Neuroscience, and the recent joint PhD program in Health Sciences in Engineering with the Rensselaer Polytechnic Institute. This structure allows students to earn a specific concentration or specialization notation on their transcripts by completing a minimum of six credits in concentration-related elective courses, in addition to the required courses and a thesis or capstone project in concentration-related fields.
Students can choose from nine specialty areas to tailor their studies, including:
- Cancer Biology
- Disease Mechanisms and Therapeutics
- Development, Regeneration, and Stem Cells
- Immunology
- Genetics and Genomics
- Microbiology
- Neuroscience
- Artificial Intelligence and Emerging Technologies in Medicine
- Health Sciences in Engineering
Visit our website or contact us to learn more about this program and find out which track aligns with your schedule and career goals.